Mpox (Monkeypox)
We are updating webpages with the term “mpox” to reduce stigma and other issues associated with prior terminology. This change is aligned with the recent World Health Organization decision.
Vaccination sites for people who are eligible for a JYNNEOS vaccine:
Pharmacies
- Longs Drug (CVS) Pharmacies:
- Schedule online at https://www.cvs.com/immunizations/get-vaccinated
- Walgreens Pharmacies:
- Schedule online at https://www.walgreens.com/findcare/schedule-vaccine
Vaccine Clinics
Appointments are required for all clinics except where noted.
- Oahu residents can contact:
- Hawai’i Health & Harm Reduction Center (in Honolulu) at 808-521-2437
- Kaiser Permanente, Mapunapuna Medical Office (in Honolulu) at 808-432-2000
- Waikiki Health at 808-922-4787
- Kauai residents can contact:
- Malama Pono Health Services (in Lihue) at 808-246-9577
- Maui residents can contact:
- Malama I Ke Ola Health Center (in Wailuku) at 808-871-7772
- Hawaii Island residents can contact:
- Hamakua-Kohala Health Centers (in Honoka’a) at 808-930-2751
- Kumukahi Health + Wellness (in Hilo and Kona) at 808-982-8800
If you are a healthcare provider and want to report a mpox case, please call our disease reporting line at 808-586-4586.
Hawaii Mpox Case Data by County of Diagnosis
6
Hawaii
38
Honolulu
4
Kauai
2
Maui
5
Out of State
55
Total
Last Updated: Thursday, October 31, 2024. Cases reported in Hawaii include three non-residents diagnosed in Kauai county and three non-residents diagnosed in Honolulu county.
Report a Case
Disease Reporting Line:
(808) 586-4586
About This Disease
Mpox (previously called monkeypox) is a contagious disease caused by the mpox virus. There are two different types of mpox virus, clade I and clade II. Though epidemiologic investigations continue, clade I historically has caused a higher percentage of people with mpox to get severely sick or die compared to clade II.
An outbreak of clade I mpox is currently occurring in the Democratic Republic of the Congo (DRC) and has been declared a Public Health Emergency of International Concern. Clade I mpox has not been identified in the United States, but health officials are continuing to monitor the situation.
In 2022-2023, an outbreak of clade II mpox occurred in the U.S. and other countries where this infection had rarely been seen. Since 2023, clade II mpox has continued to spread and sicken a small number of people throughout the U.S.
While clade II mpox infection is not usually lethal, some mpox deaths have occurred in the U.S. Even when mpox is not lethal, people can experience severe illness. Most people have not been hospitalized and have recovered on their own.
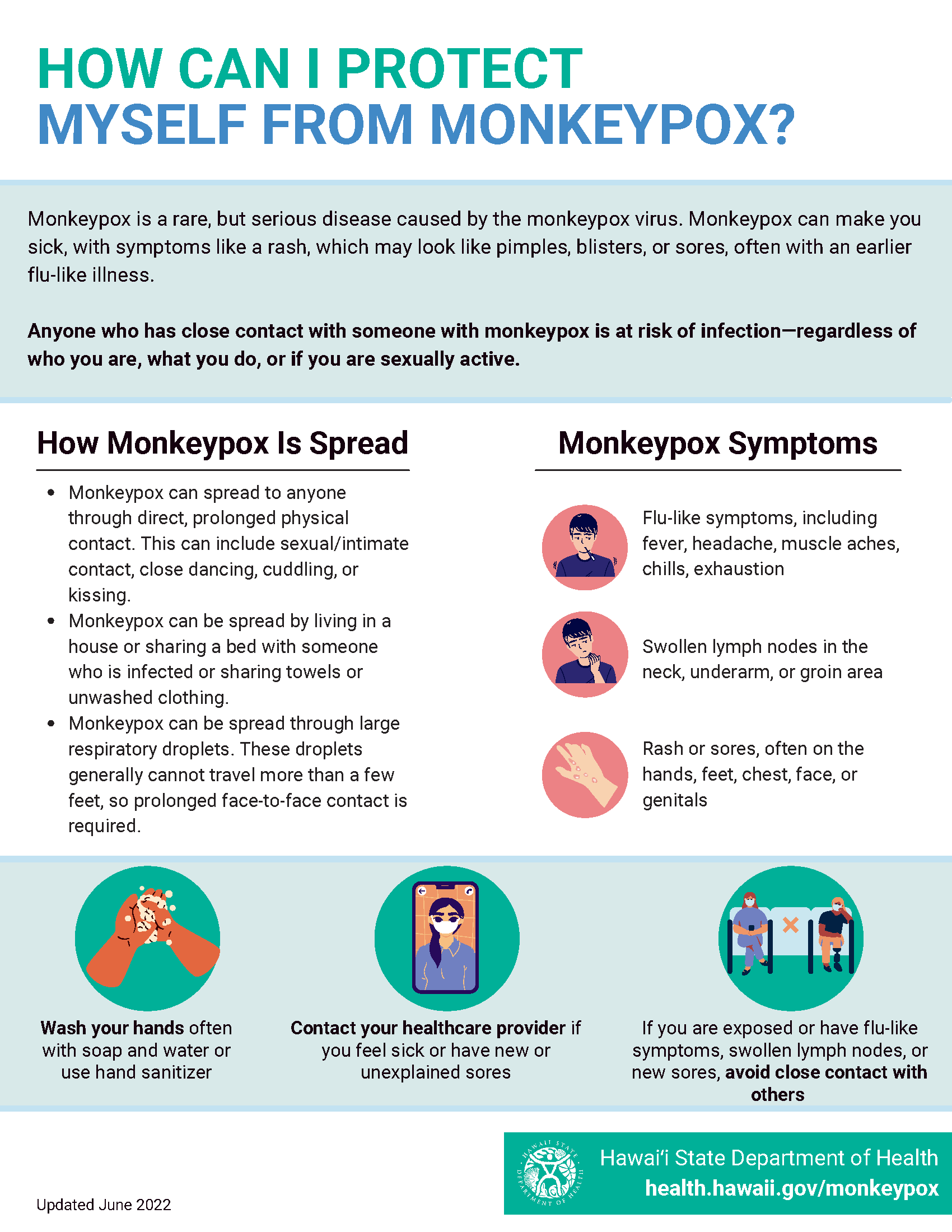
- Mpox can spread when a person comes into close, intimate contact with the virus from an infected person or materials contaminated with the virus.
- Common symptoms include flu-like symptoms; swelling of lymph nodes; rash or sores on the hands, feet, chest, face, or genitals.
- Avoid skin-to-skin and prolonged close contact (touching sores, kissing, sex) with anyone who has an unusual rash or mpox symptoms.
People exposed to mpox should contact their healthcare provider immediately. Options are available to prevent infection after high-risk close contact.
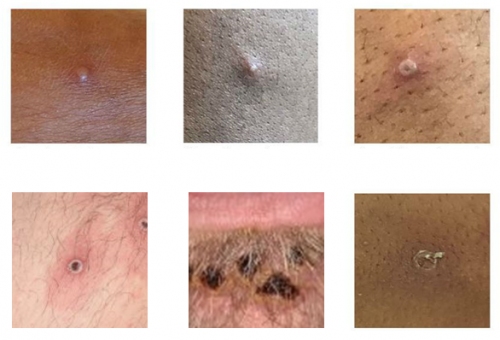
Examples of mpox lesions
Photo credit: CDC, UK Health Security Agency, World Health Organization
Infection begins with flu-like symptoms such as fever, headache, muscle aches, chills, exhaustion and swollen lymph nodes. Infection progresses to a rash or sores, often on the hands, feet, chest, face, or genitals. Individuals generally become ill within 21 days of exposure. Get the facts about mpox here.
Infections generally last two to four weeks. Individuals are infectious until all lesions are scabbed over and new skin has grown.
While most people diagnosed with mpox experience mild to moderate illness, the rash and sores can be itchy and painful. Treatment for mpox is available but must be coordinated through DOH and a physician.
Transmission can occur through:
- Direct, prolonged contact with body fluids, lesion material, or items used by someone with mpox.
- Large respiratory droplets. These droplets are spread when people breathe, cough, sneeze, or talk. These droplets generally cannot travel more than a few feet, so prolonged face-to-face contact is required.
- Close, prolonged contact with an infected person or animal.
- Sharing a bed with someone who is infected or by sharing items like towels or unwashed clothing.
- Having intimate contact with others, including during sex, kissing, cuddling, or touching parts of the body with mpox sores. At this time, it is not known if mpox can spread through semen or vaginal fluids.
- Mpox has not been proven to spread through touching items like doorknobs or by walking past someone who is infected.
Mpox is diagnosed through laboratory testing. DOH’s State Laboratories Division and commercial labs can test for orthopoxvirus. Confirmatory testing for mpox must be performed by the CDC.
Providers should refer to DOH’s August 1st medical advisory for more information on diagnosing mpox.
Additional testing resources:
Vaccination & Treatment
A vaccine for mpox called JYNNEOS is commercially available and has FDA approval for persons 18 years of age and older and authorization for persons younger than 18 years for the prevention of mpox for those who are at high risk for infection. The CDC recommends vaccination with the 2-dose JYNNEOS vaccine series for persons who are at risk for mpox. The vaccine is covered by Medicare, Medicaid, and most private insurance plans for individuals at risk for mpox.
JYNNEOS vaccine reduces a person’s chance of getting mpox and may reduce symptoms if they are already infected. No vaccine is 100% effective, so vaccinated individuals should still try to reduce their risk of exposure to mpox both before and after getting the JYNNEOS vaccine.
JYNNEOS is given as a series of two doses given at least 28 days (4 weeks) apart. People need to get both doses of the vaccine for the best protection against mpox.
Most people who get the JYNNEOS vaccine have minor reactions. These may include pain, redness, swelling, firmness, or itching where the shot was given. Other symptoms that can occur after vaccination include muscle pain, headaches, nausea, chills, or feeling tired. There is a small chance of fever.
When JYNNEOS vaccine is given intradermally, some people have reported less pain after vaccination but more side effects like itching, swelling, redness, thickening of the skin, and skin discoloration at the spot where the vaccine was given. Some of these side effects may last for several weeks. If you have concerns about receiving the vaccine intradermally, you can ask for the vaccine to be given to you subcutaneously in the fat layer underneath the skin on the back of your upper arm (triceps).
Like with any medicine, there is a very small chance of a vaccine causing a severe allergic reaction. If you have signs of a severe allergic reaction (such as hives, swelling of the face or throat, difficulty breathing, a fast heartbeat, or dizziness), call 911 immediately or go to the nearest hospital. For other concerns, contact a health care provider.
-
- Adverse reactions should be reported to the Vaccine Adverse Event Reporting System (VAERS). Your health care provider will usually file this report, or you can do it yourself. Visit the VAERS website or call 800-822-7967. VAERS is only for reporting reactions, and VAERS staff members do not give medical advice.
- You can visit the FDA website (PDF) to read the package insert for this vaccine. For more information on the vaccine, visit the CDC JYNNEOS Vaccine Statement (PDF) and the CDC’s Mpox Vaccination Site.
Those who should consider getting vaccinated against mpox include individuals who meet the following criteria:
Parental consent is required for vaccination of individuals under 18 years of age. Workers in certain occupational groups are also eligible: Clinical laboratory personnel performing diagnostic testing for orthopoxviruses and research laboratory personnel who directly handle cultures or animals contaminated or infected with orthopoxviruses (see ACIP recommendations). |
Pharmacies
- Longs Drug (CVS) Pharmacies:
- Schedule online at https://www.cvs.com/immunizations/get-vaccinated
- Walgreens Pharmacies:
- Schedule online at https://www.walgreens.com/findcare/schedule-vaccine
Vaccine Clinics
- Oahu residents can contact:
- Hawai’i Health & Harm Reduction Center (in Honolulu) at 808-521-2437
- Kaiser Permanente, Mapunapuna Medical Office (in Honolulu) at 808-432-2000
- Waikiki Health at 808-922-4787
- Kauai residents can contact:
- Malama Pono Health Services (in Lihue) at 808-246-9577
- Maui residents can contact:
- Malama I Ke Ola Health Center (in Wailuku) at 808-871-7772
- Hawaii Island residents can contact:
- Hamakua-Kohala Health Centers (in Honoka’a) at 808-930-2751
- Kumukahi Health + Wellness (in Hilo and Kona) at 808-982-8800
Nationwide, the current cases are primarily spreading among social networks of gay, bisexual and other men who have sex with men. However, anyone who has been in close contact with someone with mpox is at increased risk of infection, regardless of a person’s gender, sexual orientation, or travel history.
If you are at increased risk for mpox, you may want to postpone having new casual sex partners and avoid events where you have close bodily contact with others, at least during the current outbreak.
If you have symptoms consistent with mpox or have an unusual rash or sores, avoid close contact with others. Contact your healthcare provider and let them know ahead of an appointment that you may have been exposed to mpox.
Practice proper hand hygiene regularly. Washing your hands with soap and water for at least 20 seconds helps prevent the spread of disease, including mpox.
While mpox infection is generally not lethal, people can experience severe outcomes. Treatment for mpox is available but must be coordinated through DOH and a physician.
Guidance
About the Disease
Mpox is a rare, but serious disease caused by the mpox virus. It can be spread from infected humans, animals, and materials contaminated with the virus. While generally less severe and much less infectious than smallpox, mpox can be a serious illness.
The risk to most Hawaii residents remains low. Anyone who has direct skin-to-skin or prolonged close contact with someone with mpox is at risk of infection—regardless of who they are, what they do, or if they are sexually active.
Nationwide and in Hawaii, mpox cases have been disproportionately reported among social networks of gay or bisexual men, or other men who have sex with men. While many of those affected in the current outbreaks identify as gay or bisexual, anyone who had direct skin to skin or prolonged close contact with someone with mpox is at risk of infection.
Infection begins with flu-like symptoms such as fever, headache, muscle aches, chills, exhaustion, and swollen lymph nodes. Infection progresses to a rash or sores, often on the hands, feet, chest, face, or genitals. Individuals generally become ill within 21 days of exposure. People may have all of the symptoms or only a few.
Yes, vaccines can prevent disease or reduce the severity of mpox disease. If administered after exposure to mpox , vaccines work best when administered within 4 days.
Yes, treatment is available, but it must be coordinated through your healthcare provider and DOH. If you think you’ve been exposed to mpox or have symptoms of mpox, call your healthcare provider and notify them of your situation. Read more here.
Mpox is diagnosed through laboratory testing. Your healthcare provider can order testing.
Transmission
Mpox is primarily spread from person to person through close, prolonged physical contact. It is much harder to spread than COVID-19, colds, or the flu.
- Mpox can be spread through direct skin-to-skin or prolonged close contact with someone who has mpox. This can include sexual/intimate contact, cuddling, or kissing while a person is infected.
- Mpox can spread by sharing a bed with someone who is infected or by sharing items like towels or unwashed clothing.
- Mpox can spread through large respiratory droplets. These droplets generally cannot travel more than a few feet, so prolonged face-to-face contact is required.
- Mpox has not been proven to spread through touching items like doorknobs or by walking past someone who is infected.
A person with mpox is infectious from the time symptoms start to when the rash has fully healed and a new layer of skin has formed. Mpox typically lasts 2-4 weeks. People who do not have mpox symptoms cannot spread the virus to others.
There are a number of simple steps you can take to help prevent getting infected with mpox.
- Get vaccinated if you are at risk of mpox
- Reduce your risk of mpox during sex or social gatherings where there is direct, personal, skin-to-skin contact
- Avoid close, skin-to-skin contact with people who have a rash that looks like mpox and animals that carry the mpox virus
- Avoid contact with objects and materials that a person with mpox has used
- Wash your hands often
Mpox can spread through close contact (including intimate or sexual contact) with a person with mpox, through contact with contaminated materials, and through direct contact with infected wild animals. Mpox can spread during sex by:
- Oral, anal, and vaginal sex, or touching the genitals or anus of a person with mpox
- Hugging, massaging, kissing, or talking closely
- Touching fabrics, shared surfaces, and objects, such as bedding, towels, and sex toys, that were used by a person with mpox
Individuals who have symptoms consistent with mpox should contact their healthcare provider. Make sure to call ahead and mention that you may have been exposed to mpox.
Contact your healthcare provider and let them know that you are a close contact. Your healthcare provider can work with DOH to arrange testing and vaccination if appropriate.
Mpox can spread through direct, prolonged skin-to-skin contact with someone who has mpox symptoms.
Personal service providers should consider asking clients about any new or unexplained rash or sores and take precautions.
Nationwide and in Hawaii, mpox cases have been disproportionately reported among social networks of gay or bisexual men, or other men who have sex with men. While many of those affected in the current outbreaks identify as gay or bisexual, the risk of mpox is not limited to people who are sexually active or men who have sex with men.
Vaccination
Those who should consider getting vaccinated against mpox include individuals who meet the following criteria:
- Gay, bisexual, and other men who have sex with men, as well as transgender or nonbinary people who in the past 6 months have had one or more of the following:
- A new diagnosis of 1 or more sexually transmitted infections
- Multiple or casual sex partners (e.g., such as through dating apps)
- People who have a sex partner in any of the categories described above
- People who anticipate experiencing any of the above
- Anyone with close contact in the last 14 days to a person with known or suspected mpox infection
- Travelers to a country with a clade I mpox outbreak who anticipate any of the following activities during travel, regardless of gender identity or sexual orientation:
- Sex with a new partner
- Sex at a commercial sex venue (e.g., a sex club or bathhouse)
- Sex in exchange for money, goods, drugs, or other trade
- Sex in association with a large public event (e.g., a rave, party, or festival)
- Anyone in any of these categories who has only received one vaccine dose
Parental consent is required for vaccination of individuals under 18 years of age.
Workers in certain occupational groups are also eligible: Clinical laboratory personnel performing diagnostic testing for orthopoxviruses and research laboratory personnel who directly handle cultures or animals contaminated or infected with orthopoxviruses (see ACIP recommendations).
- Most people who get the JYNNEOS vaccine have minor reactions. These may include pain, redness, swelling, firmness, or itching where the shot was given, especially for intradermal injection (between layers of the skin). Some people have reported reactions lasting 2-4 weeks, or longer.
- You also may have muscle pain, headaches, nausea, chills, or may feel tired. There is a small chance of fever. As with any medicine, there is a very small chance of a vaccine causing a severe allergic reaction.
- If you have signs of a severe allergic reaction (such as hives, swelling of the face or throat, difficulty breathing, a fast heartbeat, or dizziness), call 911 immediately or go to the nearest hospital. For other concerns, contact a health care provider.
- Adverse reactions should be reported to the Vaccine Adverse Event Reporting System (VAERS). Your health care provider will usually file this report, or you can do it yourself. Visit the VAERS website or call 800-822-7967. VAERS is only for reporting reactions, and VAERS staff members do not give medical advice.
- You can visit the FDA website (PDF) to read the package insert for this vaccine. For more information on the vaccine, visit the CDC JYNNEOS Vaccine Statement (PDF) and the CDC’s Consideration on Mpox Vaccine site.
Mpox Infection Prevention Guidelines for Hotels and Dorms/University Housing
CONTACT TRACING
If you are notified of a case or HDOH is aware of a case, we will be working with you on contact tracing and offering guidance as needed.
CLEANING, DISINFECTING AND LAUNDRY
Avoid activities that could spread dried material from lesions (e.g., use of fans, dry dusting, sweeping, or vacuuming) in these areas. Perform disinfection using an EPA-registered disinfectant with an Emerging Viral Pathogens claim, which may be found on EPA’s List Q. Follow the manufacturer’s directions for concentration, contact time, and care and handling.
Linens can be laundered using regular detergent and warm water. Soiled laundry should be gently and promptly contained in a laundry bag and never be shaken or handled in a manner that may disperse infectious material. Covering mattresses in isolation areas (e.g. with sheets, blankets, or a plastic cover) can facilitate easier laundering.
ISOLATION
Isolate staff, volunteers, or students who have mpox away from congregate settings until they are fully recovered. Flexible, non-punitive sick leave policies for staff members are critical to prevent spread of mpox.
Reduce the number of staff who are entering the isolation areas to staff who are essential to isolation area operations.
PERSONAL PROTECTIVE EQUIPMENT (PPE)
Cleaning and disinfection—Staff, volunteers, or residents should wear a gown, gloves, eye protection, and a well-fitting mask or respirator when cleaning areas where people with mpox spent time.
Laundry—When handling dirty laundry from people with known or suspected mpox infection, staff, volunteers, or residents should wear a gown, gloves, eye protection, and a well-fitting mask or respirator. PPE is not necessary after the wash cycle is completed.
ADDITIONAL RESOURCES:
- CDC Mpox Print Resources
- CDC Mpox for Congregate Settings
HOTELS
- American Hotel & Lodging Association “Safe Stay” What Hotels Should Know About Monkeypox
COLLEGES DORMS/UNIVERSITY HOUSING
- Cornell Health Monkeypox: What To Know
- UCI Environmental Health & Safety. Cleaning Guidance for Student Housing in Response to Monkeypox
Specimen Collection for Mpox Diagnosis One-Pager
Recommended Personal Protective Equipment
Infection Prevention and Control of Mpox in Healthcare Settings
June 3 DOH Medical Advisory: Probable Case of Mpox Identified in Hawaii
August 1 DOH Medical Advisory: Diagnosis, Management and Prevention of Mpox Virus Infection
August 15 DOH Medical Advisory: Update—Mpox Virus Vaccination Recommendations
CDC Information for Healthcare Professionals
Cleaning and Disinfection Practices
Resources
Mpox Informational Video: Hot Pot Podcast
Mpox and Gay and Bisexual Men: Fact Sheet