Announcements
🚧 Website modernization in progress. Mahalo no kou ʻae ʻana.
📢📘🚁 EMSIPSB Reports to Legislature – 2026 Regular Session
2025-2026 Aeromedical Services Working Group Report – Pursuant to Senate Concurrent Resolution 86 (SCR 86) 2025.
Trauma System Special Fund Legislative Report FY2025
Emergency Medical Services (EMS) Special Fund Legislative Report FY2025
🚁🏥🚁 Hawaii Air Medical Resource Tracking Board for Hospitals
Below are links to the rollout webinar in partnership with Healthcare Association of Hawaii (HAH), along with direct link to the Air Medical Resource Tracking Board, and pdf resource guide to understand the data being reported by air medical providers.
Request Access to view the Air Medical Resource Tracking Board Recorded Webinar.
View the Live Hawaii Air Medical Resource Tracking Board Guide for Hospitals
View the Live Hawaii Air Medical Resource Tracking Board
🏥🚁🚑 EMS and Hospital Facility Identifier Update and Master List Request Form
Support Note: EMS agencies, hospitals, and registry users who experience issues with system Insight Reports related to the master identifier list implementation should submit an email request directly to Logan Diehl at [email protected] and cc the email copy to EMSIPSB at [email protected]
EMS and Hospital Facility Identifier Update and Master List Request Form.
View EMS and Hospital Facility Identifier Master List Rollout Webinar PowerPoint
View Live Webinar Recording until January 8, 2026
🏥 Rural Healthcare Transformation Program Proposals
View RHTP Proposal Worksheet
View RHTP Budget Worksheet
View RHTP Powerpoint
📕🏥 ACS Resources for Optimal Care of Injured Patient
View ACS Standards
🚁 New Air‑Medical Event Reporting Form – Now Live
Open the Air Medical Event Reporting Form
🚑📈 2025 Standing Orders & Correction Memo – Available
Download PDF
🚑📈 2025 Standing Orders Presentation
View Presentation
📢📘 EMS Measles Response Bulletin
Download Bulletin
🌊⚠️🏊 2025 Hawaii Water Safety Plan
View Plan
💸🗂️ EMS Contractors Report of Expenditures
Download Report
🏥⚕️📢 Trauma System Resources Submission Form
Open Submission Form
🏥⚕️📘 Hawaii Trauma Transfer Guide
Download Guide
Statewide EMS Calls Year-to-date
Statewide EMS Confirmation of Invasive Airway
Statewide EMS YTD KPI of documented EtCO2.
National Median 66.7% National Top Box 87.5% or Higher.
N=1,281 Invasive Airways N=1,012 with waveform EtCO2
Performance Improvement & Patient Safety
Statewide Trauma Registry Encounters Year-to-date
Performance Improvement & Patient Safety
Mission Zero Preventable Deaths
Statewide Trauma Registry Deaths Year-to-date
Performance Improvement & Patient Safety
Mission Zero Preventable Deaths
Mortality Rate
Statewide Trauma Registry Mortality Rate Year-to-date
Target Less Than National Mortality Benchmark of 4.39%
as published by American College of Surgeons
Trauma Quality Improvement Program (TQIP)
Performance Improvement & Patient Safety
Statewide Average EMS Scene Time for Trauma
KPI Threshold Less Than 20 Minutes.
Statewide EMS Ambulance Patient Offload Time (APOT)
State of Hawaii is ranked in 90th Percentile. 90% of all APOT events are offloaded within 17:55.
Median for the State is 5:20; half of all patients are offloaded within 5:20 at a hospital or ED.
Average 911 EMS Response Time
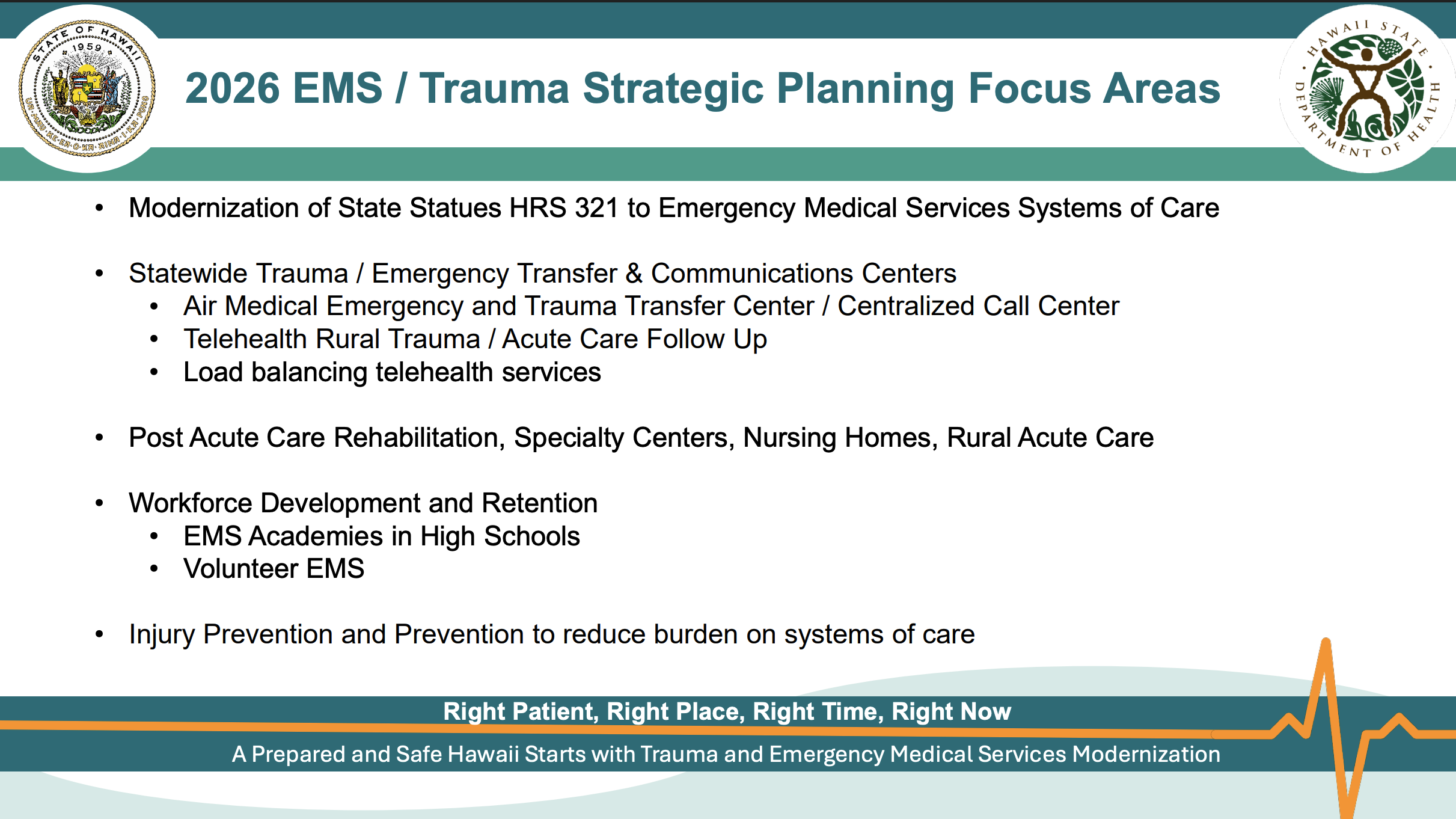
Journey to Modernize Emergency Medical Services (EMS) into Hawaii’s Emergency Medical Systems of Care
In Hawaii, the Emergency Medical Services (EMS) System and the Injury Prevention and Control System originally operated under separate branches of the Department of Health. In 2008, they merged to form the Emergency Medical Services and Injury Prevention Systems Branch (EMSIPSB). Since 2015, this partnership has evolved into a strategic, data‑driven collaboration.
In 2024, EMSIPSB spearheaded data modernization across acute care networks, 911 communications, and air‑medical transport—identifying critical puka (gaps) and enabling faster, more coordinated responses.
Now, in 2025, we’re setting out on a journey to building a unified, resilient emergency medical systems of care network founded on six critical pillars: Injury Prevention, Emergency Medical Services (EMS) & First Responders, Acute Care Systems, Quality / Performance Improvement and Patient Safety, Emergency Preparedness, and Systems Integration. By weaving together dispatch, pre‑hospital care, hospital-based teams, surgical specialists, and post‑acute rehabilitation, our Emergency Medical Systems of Care will ensure every patient journey is seamless, efficient, and life‑saving.
1. Injury Prevention
Reducing preventable injuries through data-driven education & upstream interventions.
2. EMS & First Responders
Strengthening prehospital care, field triage, & 911 coordination.
3. Acute Care Systems
Coordinating trauma, stroke, cardiac, burn & specialty centers statewide.
4. Quality & Patient Safety
Implementing CQI frameworks with real-time data & standards.
5. Emergency Preparedness
Ensuring readiness for disasters, mass casualty & public health emergencies.
6. Systems Integration
Advancing interoperability across EMS, hospitals & public health.
Our Mission: Nā Lawelawe Ola
(The Servants of Life)
Is to protect, promote, and deliver critical time-sensitive community centered pre-hospital, emergency, trauma, and acute-care services where and when they are needed most for our island’s public health and safety.
Our Vision: Making A Difference
By advancing modern data, clinical, and community care practices that enhance prevention, preparedness, education, access, and quality care from time-sensitive critical events through recovery.