Pertussis (Whooping Cough)
Report a Case
Disease Reporting Line:
(808) 586-4586
What to Know
- In 2024-2025, Hawai‘i is experiencing a worrying rise in pertussis (whooping cough) cases statewide.
- As of July 31, 2025, a total of 203 cases of pertussis – more than double the 84 cases identified in all of 2024.
- Cases have been reported in every county, with the highest rates on Kaua‘i, Maui, and Hawai‘i Island. Infants under 1 year old have been the most severely affected group.
- In addition, there are elevated case rates being seen among toddlers, children and adolescents.
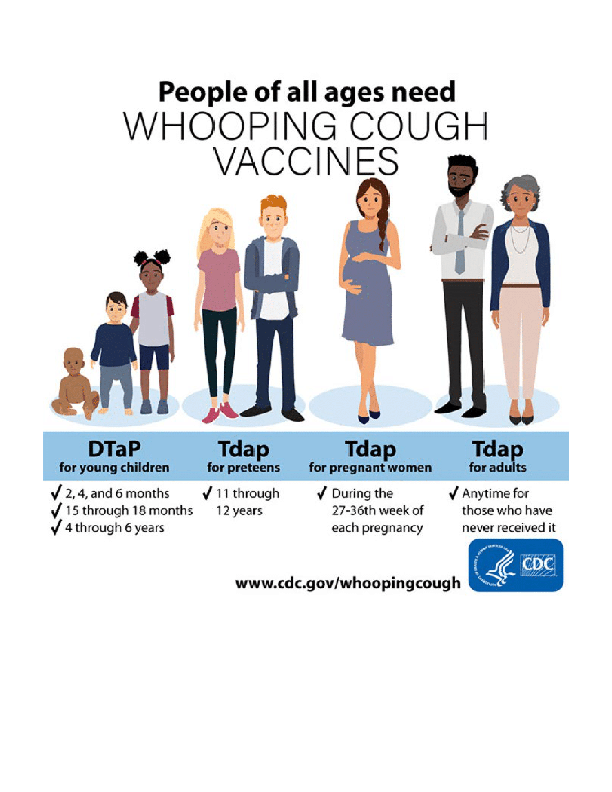
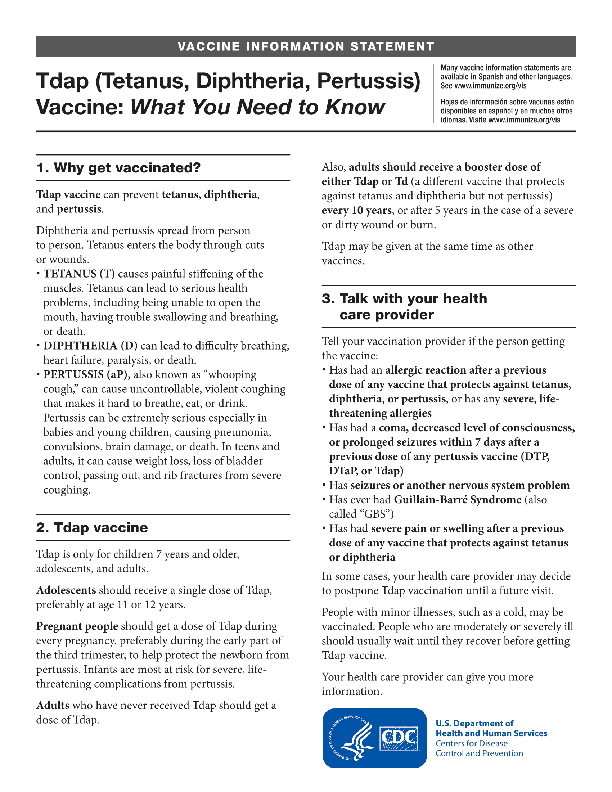
- The most effective way to reduce the risk and severity of pertussis is through vaccination with either the DTaP (diphtheria, tetanus and pertussis) or Tdap (tetanus, diphtheria and pertussis) vaccines. DTaP has been in use for more than 30 years, and the first dose is recommended at 2 months of age.
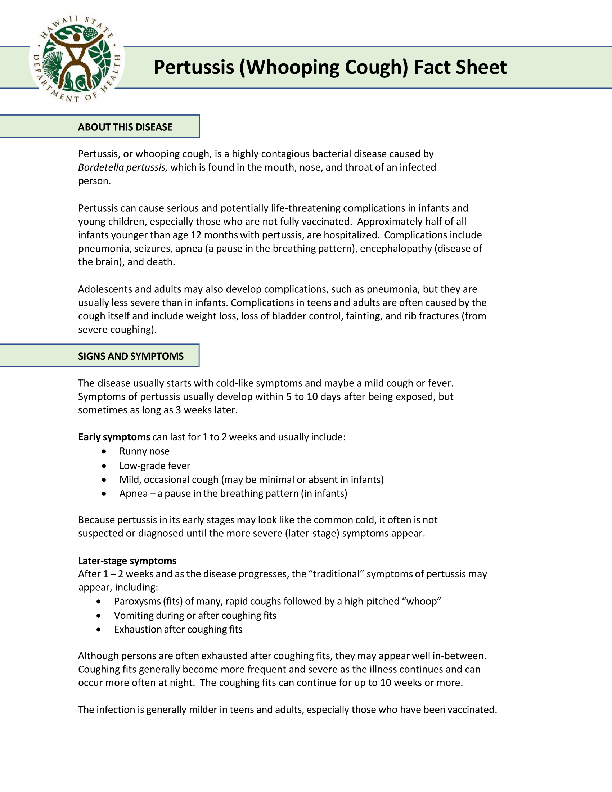
About This Disease
Whooping cough, also known as pertussis, is a very contagious respiratory illness caused by the bacteria Bordetella pertussis. Pertussis bacteria is found in the mouth, nose, and throat of an infected person and is spread person to person through droplets produced during coughing, sneezing or close contact. Adults and older children often spread pertussis unknowingly to infants. People can get pertussis at any age.
Pertussis can cause serious and potentially life-threatening complications with infants and young children, especially those who are not fully vaccinated. Approximately half of all infants younger than age 12 months with pertussis, are hospitalized. Complications include pneumonia, seizures, apnea (a pause in the breathing pattern), encephalopathy (disease of the brain), and death.
Adolescents and adults may also develop complications, such as pneumonia, but they are usually less severe than in infants. Complications in teens and adults are often caused by the cough itself and include weight loss, loss of bladder control, fainting, and rib fractures (from severe coughing).
Current Events
Pertussis in the United States
In the United States, reports of pertussis cases were than lower usual during and immediately after the COVID-19 pandemic. Since then, more than 10,000 cases are typically being reported each year returning to pre-pandemic patterns. Preliminary data show that more than six times as many cases were reported in 2024 compared to 2023.
In 2025, reported cases of pertussis have been trending down since a peak in November 2024. However, preliminary case report numbers remain elevated in 2025 compared to immediately before the pandemic.
Pertussis in Hawai‘i 2025
As of July 31, 2025, the state of Hawai‘i continues worrisome rise in pertussis (whooping cough) cases and has identified 203 case of pertussis – more than double the 84 cases identified in all of 2024.
Department of Health (DOH) issued a medical advisory to providers and a news release to inform the public of increase of pertussis cases across all the Hawaiian islands. Cases have been reported in every county, with the highest rates on Kaua‘i, Maui, and Hawai‘i Island. Infants under 1 year old have been the most severely affected group. In addition, there are elevated case rates being seen among toddlers, children and adolescents.
Why is this a public health concern in Hawai‘i?
Pertussis is a highly contagious respiratory disease spread through the air via coughs or sneezes of an infected person. Initially, the symptoms resemble a cold but can progress to intense coughing fits. In children, coughing fits can be followed by a deep breath that makes a “whooping” sound. Health complications can be serious and even life-threatening, especially for infants and young children who are not fully vaccinated. Complications include pneumonia, seizures, apnea (a pause in breathing), encephalopathy (a disease of the brain) and death.
The most effective way to reduce the risk and severity of pertussis is through vaccination with either the DTaP (diphtheria, tetanus and pertussis) or Tdap (tetanus, diphtheria and pertussis) vaccines. DTaP has been in use for more than 30 years, and the first dose is recommended at 2 months of age. Tdap has been available for nearly 20 years and is recommended for pregnant women which helps protect their newborns as well as for adolescents and adults. See the DOH pertussis webpage for more details.
The DOH continues to work closely with families, healthcare providers and schools to identify close contacts of cases, recommend testing, treatment when appropriate, and support public health measures to reduce further spread of pertussis.
Signs and Symptoms
The disease usually starts with cold-like symptoms and maybe a mild cough or fever. It primarily affects the lungs and airways and is known for its severe, uncontrollable coughing fits, which can make breathing difficult. The cough is often followed by a high-pitched “whoop” sound as the person tries to inhale. Fever is generally minimal throughout the course of the illness. Symptoms of pertussis usually develop within 5 to 10 days after being exposed, but sometimes as long as 3 weeks later.
Early symptoms can last for 1 to 2 weeks and usually include:
- Runny nose
- Low-grade fever
- Mild, occasional cough (may be minimal or absent in babies)
- Apnea – babies may struggle to breathe, resulting in a pause in the breathing pattern
Because pertussis in its early stages may look like the common cold, it often is not suspected or diagnosed until the more severe (later-stage) symptoms appear.
Later-stage symptoms
After 1–2 weeks and as the disease progresses, the “traditional” symptoms of pertussis may appear, including:
- Paroxysms (fits) of many, rapid coughs followed by a high-pitched “whoop” sound
- Vomiting during or after coughing fits
- Exhaustion after coughing fits
Although persons are often exhausted after coughing fits, they may appear fairly well in-between. Coughing fits generally become more frequent and severe as the illness continues and can occur more often at night. The coughing fits can continue for up to 10 weeks or more.
The infection is generally milder in teens and adults, especially those who have been vaccinated.
Transmission
Pertussis spreads through the air by respiratory droplets when an infected person coughs or sneezes while in close contact with others, infecting someone who breathes in the pertussis bacteria. It is spread to those with prolonged close contact with an infected person or share breathing space, such as a household member. Anyone at any age can get pertussis.
People who have pertussis, who do not take antibiotics can spread the disease during the first three weeks they are coughing. Note: The cough will generally last longer than three weeks until the lungs are healed.
People who have pertussis, who complete five days of affective antibiotics can no longer spread the disease (full course of antibiotics should be completed).
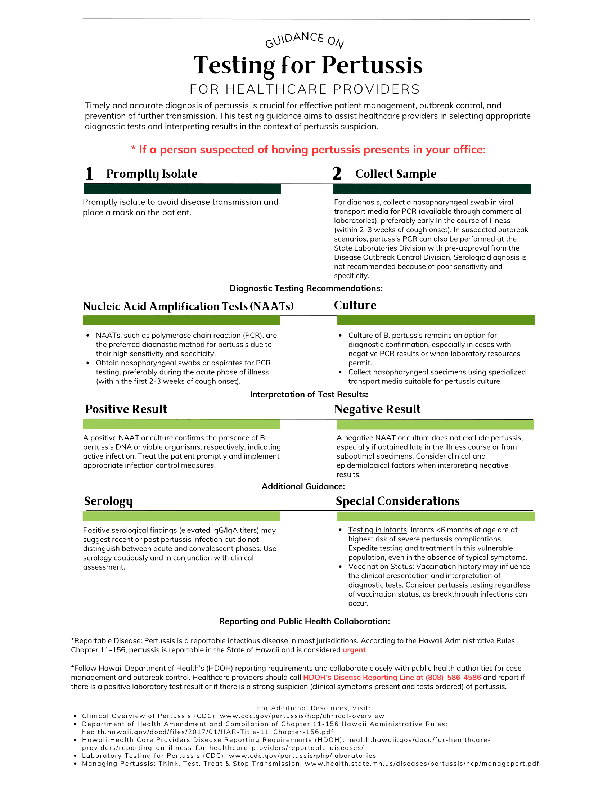
Diagnosis
Pertussis is diagnosed by a combination of symptoms, signs, physical examination, and laboratory tests. People with symptoms of pertussis or who have been exposed to someone with pertussis should contact a healthcare provider immediately.
Treatment
Pertussis is generally treated with antibiotics. Early treatment of pertussis is very important. Treatment may make the infection less serious if it is started early, before coughing fits begin, and may help prevent the spread of pertussis to close contacts.
Treatment after three weeks of illness is unlikely to help, even though the person still has symptoms.
Persons who have been in close contact with someone with pertussis (such as household members), especially those at high risk for developing severe disease, should also receive antibiotics after exposure to try to prevent getting or spreading the disease. Close contacts should receive antibiotics regardless of their age and vaccination status.
Pertussis can sometimes be very serious, requiring treatment in the hospital. Infants are at greatest risk for serious complications from pertussis.
Risk in Hawaii
Prevention
The most effective way to prevent pertussis is through vaccination. Pertussis vaccines are recommended for people of all ages. There are two kinds of vaccines used today to protect against pertussis, both of which are combined with vaccines for other diseases:
Infants and Children
- Need 5 doses of DTaP vaccine for maximum protection, at ages 2, 4, 6, 15-18 months, and at 4-6 years.
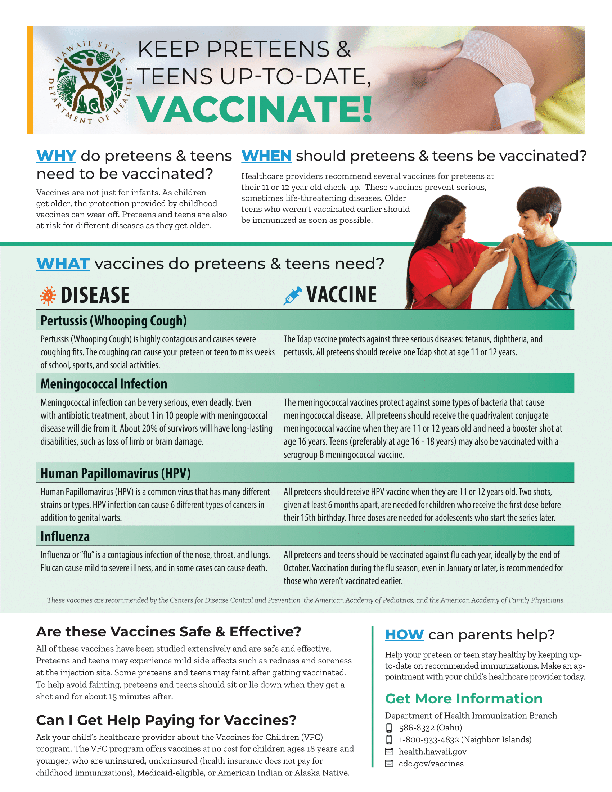
Adolescents
- Should receive a single dose of Tdap, preferably at age 11 or 12 years.
Adults
- Those who have never received Tdap should get a dose of Tdap.
- Adults should receive a booster dose of either Tdap or Td (a different vaccine that protects against tetanus and diphtheria but not pertussis) every 10 years, or after 5 years in the case of a severe or dirty wound or burn.
Pregnant Women
- They should receive a dose of Tdap vaccine during the 3rd trimester of each pregnancy, preferably during the early part of gestational weeks 27 through 36.
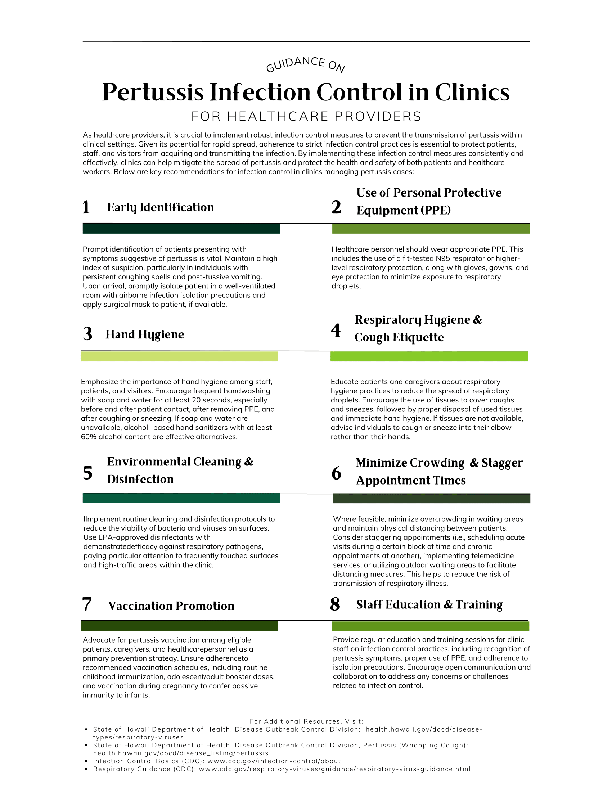
Healthcare Personnel
- Those who have direct patient contact (especially with infants) should receive a single dose of Tdap if they have not previously received one.
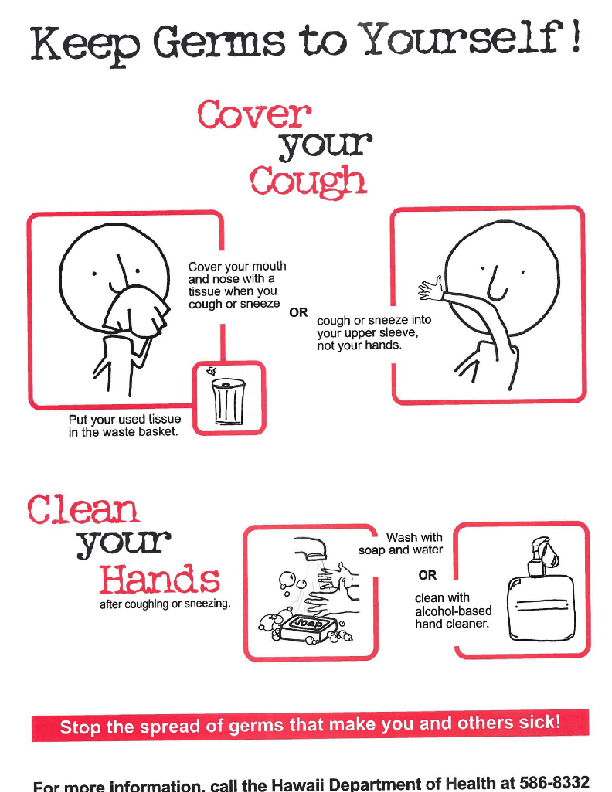
In addition to vaccination, practicing good hygiene is recommended to prevent the spread of respiratory illnesses, including pertussis. You should:
- Cover your mouth and nose with a tissue when you cough or sneeze.
- Put your used tissue in the waste basket.
- Cough or sneeze into your upper sleeve or elbow, not your hands, if you don’t have a tissue.
- Wash your hands often with soap and water for at least 20 seconds.
- Use an alcohol-based hand rub if soap and water are not available.
To provide a circle of protection around the infant until they are old enough to get all the doses of vaccine to be fully protected, DOH also encourages a “cocooning strategy” which involves ensuring close contacts of a baby, including parents, siblings, grandparents, childcare staff, caregivers and healthcare providers, are up to date on their pertussis vaccines.
Recent News
 Department of Health Responding to Increased Pertussis Cases in Hawaiʻi in 2025
Department of Health Responding to Increased Pertussis Cases in Hawaiʻi in 2025
Additional Resources
Hawaii State Department of Health
Centers for Disease Control and Prevention (CDC)
Information for Clinicians
Hawaii State Department of Health
 Pertussis Toolkit for Health Care Providers
Pertussis Toolkit for Health Care Providers
Centers for Disease Control and Prevention
 Clinical Overview of Pertussis
Clinical Overview of Pertussis
Information for Schools
- Fillable Pertussis Toolkit
- Pertussis (Whooping Cough) Fact Sheet
- School Activity Exclusion Criteria
- Purple Schools Pertussis Infographic
- Vax to School Flyer
- Protect Your Baby from Pertussis Flyer
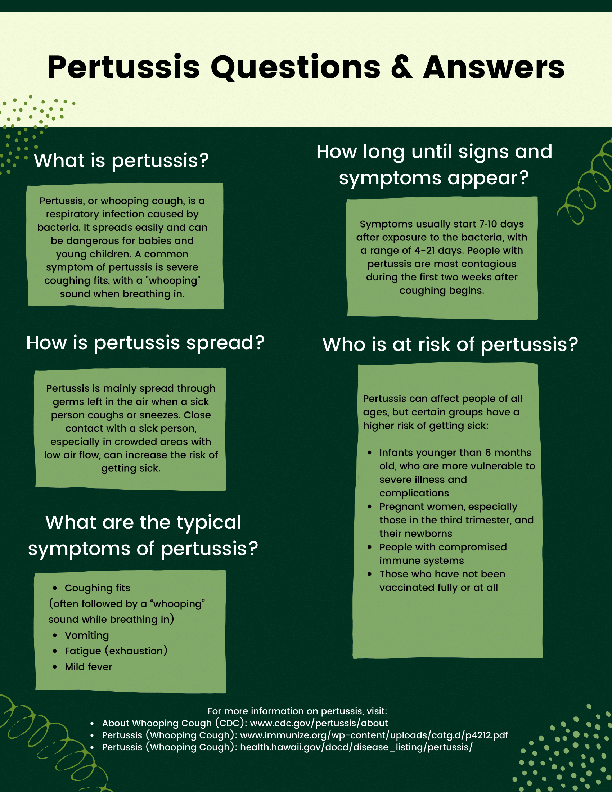
- Pertussis Questions and Answers
- Pertussis Social Media Reel
Print Materials
Disease Reporting
Pertussis is an URGENT CATEGORY NOTIFIABLE CONDITION. Healthcare providers are required to report suspected or confirmed cases of measles immediately by telephone to the Disease Investigation Branch at (808) 586-4586.
This prompt reporting is crucial for initiating timely investigations, implementing control measures, and preventing further spread of the disease. Do not wait for laboratory confirmation.
For more detailed information on reporting requirements, please refer to the Hawaii Health Care Providers Disease Reporting Requirements.
- Hawaii Administrative Rules Chapter 11-156
- Hawaii Isolation and Control Requirements | Disease Outbreak Control Division
| Disease Reporting Lines | |
|---|---|
| Oahu (Disease Reporting Line) | 808-586-4586 |
| Maui District Health Office | 808-984-8213 |
| Kauai District Health Office | 808-241-3563 |
| Big Island District Health Office (Hilo) | 808-933-0912 |
| Big Island District Health Office (Kona) | 808-322-4877 |
| After hours on Oahu | 808-600-3625 |
| After hours on neighbor islands | 808-360-2575 (toll free) |
Last reviewed November 2025