Angiostrongyliasis (Rat Lungworm)
About This Disease
Angiostrongyliasis, also known as neuroangiostrongyliasis or rat lungworm, is a disease that affects the brain and spinal cord. It is caused by a parasitic nematode (roundworm parasite) called Angiostrongylus cantonensis. The adult form of A. cantonensis is only found in rodents. However, infected rodents can pass larvae of the worm in their feces. Snails, slugs, and certain other animals (including freshwater shrimp, land crabs, and frogs) can become infected by ingesting this larvae; these are considered intermediate hosts. Humans can become infected with A. cantonensis if they eat (intentionally or otherwise) a raw or undercooked infected intermediate host, thereby ingesting the parasite. For more information on the life-cycle of A. cantonensis, visit the CDC website.

Juvenile Parmarion martensi on a nickel (credit: HDOH)

Veronicella cubensis (Credit: Rob Cowie, UH Manoa)

Achatina fulica (Credit: Jaynee Kim, Bishop Museum)
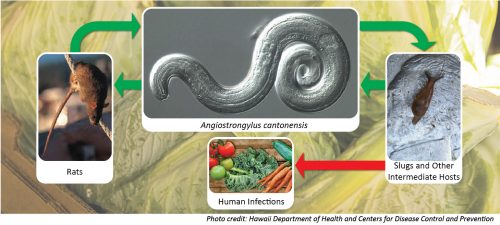
Photo credit: Hawaii Department of Health and Centers for Disease Control and Prevention
Signs and Symptoms
This infection can cause a rare type of meningitis (eosinophilic meningitis).
The clinical presentation can vary. Symptoms can start with non-specific symptoms and evolve to more specific symptoms over the next following weeks. People may experience nausea, vomiting, and abdominal pain a few hours to a few days after ingestion. Symptoms can then progress to headache and other neurologic symptoms. Non-specific symptoms include fever, light sensitivity, muscle pain, fatigue, and insomnia. More specific symptoms may include constant headache, neck stiffness and pain, tingling or burning of the skin, double vision, bowel or bladder difficulties, and seizures.
Children may experience more fever, irritability, somnolence, lethargy, gastrointestinal symptoms, muscle twitching, convulsions, and extremity weakness. In addition, individuals may experience a few days to weeks of no symptoms followed by neurologic symptoms.
Although it varies from individual to individual, the symptoms usually last between 2–8 weeks. Symptoms have also been reported to last for longer periods of time.
Transmission
You can get angiostrongyliasis by eating food contaminated by the larval stage of A. cantonensis worms. In Hawaii, these larval worms can be found in raw or undercooked snails or slugs. Sometimes people can become infected by eating raw produce that contains a small infected snail or slug, or part of one. It is not known for certain whether the slime left by infected snails and slugs are able to cause infection. Angiostrongyliasis is not spread person-to-person.
Diagnosis
Diagnosing angiostrongyliasis can be difficult, as there are no readily available blood tests.
A presumptive diagnosis is based on exposure history (such as if they have history of travel to areas where the parasite is known to be found or history of ingestion of raw or undercooked snails, slugs, or other animals known to carry the parasite), clinical signs and symptoms consistent with angiostrongyliasis, and laboratory finding of eosinophils (a special type of white blood cell) in cerebrospinal fluid (CSF).
In Hawaii, cases can confirm diagnosis with a polymerase chain reaction (PCR) test, performed by the State Laboratories Division. This type of PCR test detects A. cantonensis DNA in CSF or other tissue.
There is no reliable diagnostic test available to detect previous infections of angiostrongyliasis.
Treatment
There is no specific treatment for the disease. However, Governor Ige’s Joint Task Force on Rat Lungworm Disease published preliminary evidence-based clinical guidelines for the diagnosis and treatment of neuroangiostrongyliasis. The parasites cannot reproduce in humans and will die eventually, causing inflammation. The preliminary guidelines call for a complete neurologic examination; a detailed history of possible exposure to snails/slugs, rats, or other things suggesting a risk for infection; and a lumbar puncture, or spinal tap, to diagnose the disease and relieve headaches caused by the disease. Steroids should be given as early as possible to reduce inflammation. Anti-parasitic drugs, such as albendazole, may be helpful, although there is limited evidence of this in humans. If albendazole is used, it must be combined with steroids to treat any possible increase in inflammation caused by dying worms. Persons with symptoms should consult their healthcare provider for more information.
Risk in Hawaii
The majority of cases of rat lungworm that are identified in Hawaii have occurred on the Big Island, but cases, and infected intermediate hosts (snails and slugs), have also been identified on all of the major neighbor islands. Since the risk for infection is present statewide, the recommendations for preventing infection should be followed no matter where in the state you are.
Below are the preliminary counts of confirmed cases identified in Hawaii for 2022 and 2023. To see previous years’ counts, go here.
Number of confirmed cases of angiostrongyliasis (rat lungworm disease) during 2024:
As of April 1, 2024 (Case counts will be updated on the first working day of each month)
| Angiostrongyliasis (Rat lungworm) | Hawaii County | Honolulu County | Maui County | Kauai County | State Total |
|---|---|---|---|---|---|
| 2024 | 2 (0) | 0 | 0 | 0 | 2 (0) |
| 2023 | 4 (1) | 0 | 0 | 0 | 4 (1) |
Prevention
 To prevent angiostrongyliasis, don’t eat raw or undercooked snails or slugs, and if you handle snails or slugs, be sure to wear gloves and wash your hands. Eating raw or undercooked freshwater shrimp, land crabs and frogs may also result in infection, although, there has not been any documented cases in Hawaii. You should thoroughly inspect and rinse produce using potable water. Leaves of leafy greens should be washed one by one under running potable water. Boil snails, freshwater prawns, crabs, and frogs for at least 3–5 minutes. Only drink potable water and do not drink from garden hoses.
To prevent angiostrongyliasis, don’t eat raw or undercooked snails or slugs, and if you handle snails or slugs, be sure to wear gloves and wash your hands. Eating raw or undercooked freshwater shrimp, land crabs and frogs may also result in infection, although, there has not been any documented cases in Hawaii. You should thoroughly inspect and rinse produce using potable water. Leaves of leafy greens should be washed one by one under running potable water. Boil snails, freshwater prawns, crabs, and frogs for at least 3–5 minutes. Only drink potable water and do not drink from garden hoses.
Eliminating snails, slugs, and rats founds near houses and gardens might also help reduce risk exposure to A. cantonensis. Eliminating snails, slugs, and rats can be achieved through pesticide baits, traps, rodent proofing your home, and sanitation.
Additional Resources
2018 Legislative Report on Rat Lungworm Disease Initiatives (PDF)
Hawaii State Department of Health Rat Lungworm Fact Sheet (PDF)
Hawaii State Department of Health Rat Lung Worm Information Card (PDF)
Angiostrongyliasis (Rat Lungworm) Info Sheet (PDF)
Rodent Control Foldout Brochure (PDF)
Centers for Disease Control and Prevention (CDC) – Angiostrongyliasis
Safe Produce: Keep it Clean (Video)
CDC: What is Rat Lungworm (Angiostrongylus) Disease? (Video)
CDC: Angiostrongylus cantonensis FAQs
Education Campaign
Starting in 2017, with an appropriation from the Hawaii State Legislature, DOH launched a public information campaign to educate both residents and visitors about the risks of rat lungworm disease and how to prevent it. Products of the campaign to-date include:
- Mall advertisement (2019)
- Airport baggage claim monitors
- Television public service announcement 1
- Television public service announcement 2
- Television public service announcement 3
- Radio public service announcement 1
- Radio public service announcement 2
- Radio public service announcement 3
- Informational rack card
- Informational door hanger
- Informational poster
- Mall advertisement
- Food Safety banner (horizontal)
- Food Safety banner (vertical)
Interested persons might check with local medical providers/facilities as to the resources they may offer patients in support of the condition.
Journal Articles
Johnston D, Dixon M, Elm J, et al. 2019. Review of Cases of Angiostrongyliasis in Hawaii, 2007–2017. Am J Trop Med Hyg. (Epub ahead of print)
Qvarnstrom Y, Xayavong M, da Silva ACA, et al. 2015. Real-Time Polymerase Chain Reaction Detection of Angiostrongylus cantonensis DNA in Cerebrospinal Fluid from Patients with Eosinophilic Meningitis. Am J Trop Med Hyg. (Epub ahead of print)
Kwon E, Ferguson TM, Park SY, et al. 2013. A Severe Case of Angiostrongylus Eosinophilic Meningitis with Encephalitis and Neurologi Sequelae in Hawaii. Hawaii J Med Public Health. 72(6): 41–5
Wilkins PP, Qvarnstrom Y, Whelen AC, et al. 2013. The Current Status of Laboratory Diagnosis of Angiostrongylus cantonensis Infections in Humans Using Serologic and Molecular Methods. Hawaii J Med Public Health. 72(6): 55–7
Hochberg NS, Blackburn BG, Park SY, et al. 2011. Eosinophilic Meningitis Attributable to Angiostrongylus cantonensis Infection in Hawaii: Clinical Characteristics and Potential Exposures. Am J Trop Med Hyg. 85(4): 685–90
Hochberg NS, Park SY, Blackburn BG, et al. 2007. Distribution of Eosinophilic Meningitis Cases Attributable to Angiostrongylus cantonensis, Hawaii. Emerg Infect Dis. 13(11): 1675–80
Hollingsworth RG, Kaneta R, Sullivan JJ, et al. 2007. Distribution of Parmarion cf. martensi (Pulmonata: Helicarionidae), a New Semi-Slug Pest on Hawai‘i Island, and Its Potential as a Vector for Human Angiostrongyliasis. Pac Sci. 61(4): 457–67
Qvarnstrom Y, Sullivan JJ, Bishop HS, Hollingsworth R, da Silva AJ. 2007. PCR-Based Detection of Angiostrongylus cantonensis in Tissue and Mucus Secretions from Molluscan Hosts. Appl Environ Microbiol. 73(5): 1415–1419
Information for Clinicians
Preliminary Guidelines for the Diagnosis and Treatment of Human Neuroangiostrongyliasis (Rat Lungworm Disease) in Hawaii
 The Clinical Subcommittee of the Hawaii Governor’s Joint Task Force on Rat Lungworm Disease has published its report, “Preliminary Guidelines for the Diagnosis and Treatment of Human Neuroangiostrongyliasis (Rat Lungworm Disease) in Hawaii”. Read the full document; below are the key points of the report.
The Clinical Subcommittee of the Hawaii Governor’s Joint Task Force on Rat Lungworm Disease has published its report, “Preliminary Guidelines for the Diagnosis and Treatment of Human Neuroangiostrongyliasis (Rat Lungworm Disease) in Hawaii”. Read the full document; below are the key points of the report.
- Clinicians in Hawaii should have a high index of suspicion for neuroangiostrongyliasis.
- Suspect cases should be discussed with the Department of Health (DOH) Disease Investigation Branch (DIB) at the earliest opportunity to facilitate prompt, accurate diagnosis and appropriate patient management. Call (808) 586-4586 for the Disease Reporting Line.
- Typical symptoms in adults include severe headaches, neck stiffness, nausea, paresthesias, and limb pains. Highly suggestive symptoms include migratory hyperesthesias, cranial nerve abnormalities, ataxia, and focal neurologic findings which are migratory or do not follow a dermatomal distribution.
- Typical symptoms in children include fever, abdominal pain, vomiting, irritability, poor appetite, muscle weakness, fatigue, and lethargy.
- Lumbar puncture (LP) is an essential part of the evaluation of suspected neuroangiostrongyliasis. It is a low-risk procedure and has therapeutic benefits, including relief of headaches, nausea, and vomiting.
- A presumptive diagnosis of neuroangiostrongyliasis requires all three of the following:
- A history of suggestive symptoms and signs,
- Evidence of eosinophilic meningitis in the cerebrospinal fluid (CSF), and
- An exposure history, which includes residence in or recent travel to an endemic area.
- Eosinophilic meningitis is the hallmark of the disease and is defined as the presence of 10 or more eosinophils per μL of CSF and/or eosinophils accounting for more than 10% of CSF white blood cells when there are at least 6 total WBC per μL in CSF.
- CSF eosinophil counts may be absent or low early in the course of the disease, requiring repeat LPs if neuroangiostrongyliasis is still suspected.
- Real-time polymerase chain reaction (RTi-PCR) of CSF for A. cantonensis DNA is the best way to confirm the infection and is available in Hawaii through the DIB or from the Centers for Disease Control and Prevention (CDC) for the rest of the United States.
- CSF RTi-PCR may be negative in the early stages of infection.
- Repeat LP and testing is indicated if neuroangiostrongyliasis is still suspected.
- Baseline studies should include a complete blood count (CBC) with differential, serum electrolytes, liver function tests, renal function tests, blood glucose, urinalysis, and chest x-ray.
- Peripheral eosinophil counts of ≥ 500 cells/μL are often present during the course of the illness but may be absent.
- Magnetic resonance imaging (MRI) of the brain, although not required, may be helpful in diagnosing suspected neuroangiostrongyliasis. Focused MRI of the spine may be appropriate if indicated by clinical presentation.
- Serological tests for antibodies against A. cantonensis in the serum or CSF are not recommended for the diagnosis of neuroangiostrongyliasis.
- High dose corticosteroids have been shown to improve clinical outcomes. Start corticosteroids as soon as a presumptive diagnosis of neuroangiostrongyliasis is made and assuming no contraindications.
- Individuals with diabetes or glucose intolerance should be closely monitored.
- Modifications to the patient’s diabetes medications may be needed.
- The addition of albendazole, an anthelminthic drug, may provide additional benefits, although there is limited evidence of this in humans.
- If albendazole is used, combine with corticosteroids to blunt any possible increase in the inflammatory response to dying worms.
- Careful clinical monitoring is recommended in all patients, and specialist consultation (e.g., infectious disease, neurology, etc.) may be advisable.
- Pain management may require early consultation with a pain specialist.
Reporting
HDOH requires that clinicians report patients with eosinophilic meningitis, i.e., signs and/or symptoms consistent with meningitis plus eosinophils in the cerebrospinal fluid (CSF) without possible alternative causes, including CNS infection with other microbes, reaction to foreign material in the CNS (e.g., intracranial hardware or myelography dye), medications (e.g., intrathecal vancomycin or gentamicin), neoplasms, multiple sclerosis, and neurosarcoidosis by calling (808) 586-4586.
Resources for Clinicians
- CDC – Angiostrongyliasis Resources for Health Professionals
- Specimen Requirements for Angiostrongylus cantonensis Detection and Identification by Real-Time (RTi) Polymerase Chain Reaction (PCR) on clinical specimens
- State Laboratories Division Specimen Submission Form (81.3)
Last reviewed June 2023