Chikungunya
About This Disease
Chikungunya is a viral illness that is spread to people by mosquito bites. Chikungunya virus has been found in Africa, Asia, and Europe, and in the Indian and Pacific Oceans. In December 2013, a cluster of Chikungunya cases was identified for the first time in the Americas. Since then, chikungunya has spread throughout the Caribbean and into South and Central America. There have been several cases in Florida in 2014. None of these cases have resulted in ongoing transmission or spread of the virus. However, significant local transmission has been reported in Puerto Rico and the U.S. Virgin Islands. There has not been a locally acquired case in Hawaii to date. There are no vaccines to prevent chikungunya virus infections, and the most effective way to prevent infection is avoiding mosquito bites.

A female Aedes Aegypti mosquito
(Photo credit: Centers for Disease Control and Prevention)
Signs and Symptoms
Most people that become infected will develop some symptoms such as fever and severe joint pain in the hands and feet. Other symptoms also include headache, muscle pain, joint swelling, nausea, vomiting, redness around the eyes, or rash. The rash usually starts 2-5 days after the fever starts. Symptoms usually start about 3–7 days after being bitten by an infected mosquito. People generally recover within 7–10 days, but some people may have persistent joint pain that can last for months. Death from chikungunya is uncommon.

Posterior view of a patient’s back with a blotchy rash, captured in a clinical setting. (Photo credit: CDC)

Chikungunya rash on arm (Photo credit: PAHO/Flicker)
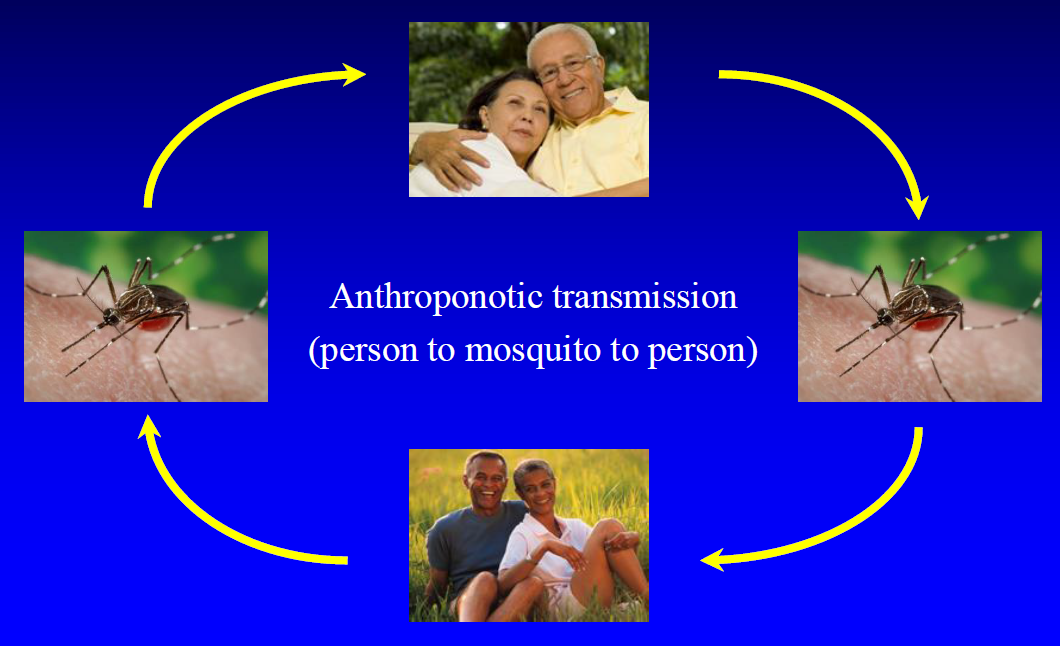
Transmission
Chikungunya is transmitted to people primarily through the bite of an infected Aedes aegypti or Aedes albopictus mosquito, the same mosquitoes that spread dengue and Zika viruses. The mosquito becomes infected when it bites a person who is already infected with the chikungunya virus. After a week or so, the mosquito is then able to infect the people it bites. Chikungunya virus cannot be transmitted from person-to-person.
Other modes of transmission that are possible but not as common are through organ transfusions, work exposure in healthcare, and from mother to baby around the time of birth.
Diagnosis
A person can be infected with chikungunya and dengue virus at the same time as they are both carried by the same types of mosquitoes. Therefore, it is important that healthcare providers consider both dengue and chikungunya when diagnosing their patients.
The diagnosis of chikungunya is based on a combination of clinical signs and symptoms, travel history, possible exposures, and testing of the blood or other body fluids. If you have symptoms of chikungunya and traveled to an area affected by chikungunya, you should contact your healthcare provider for care and evaluation. You should also stay indoors as much as possible to avoid mosquito bites and help prevent possible spread of the virus.
Treatment
There is no vaccine or specific treatments for chikungunya. Treatment is supportive. Bed rest and over the counter medication for fever and pain are recommended. Patients are advised to drink fluids to prevent dehydration. Aspirin and non-steroidal anti-inflammatory drugs (like ibuprofen) are not recommended until dengue can be ruled out to reduce the risk of bleeding. If patients are taking medicine for another medical condition, they should talk to a healthcare provider before taking additional medication.
Risk in Hawaii
Chikungunya virus is not found in Hawaii. There have been no locally acquired cases of chikungunya. All of the cases identified in Hawaii have been travel-related (or imported) and infected while outside of Hawaii. However, Hawaii’s status as a travel destination place it under continual threat of introduction of mosquito-borne diseases. Hawaii’s climate creates a year-round mosquito season. Therefore, it is important that individuals with chikungunya protect themselves from further mosquito bites during the first two weeks of illness to prevent further spread of the disease.
Prevention
The best way to prevent any mosquito-borne infections is to avoid being bitten by mosquitoes. Some steps you can take to prevent mosquito bites include:
- Applying Environmental Protection Agency (EPA) approved repellents as recommended by product label.
- Wear long pants and long-sleeved shirts when outdoors.
- Maintain screens on windows and doors.
- Empty or drain water at least weekly from garbage cans, house gutters, buckets, pool and boat covers, coolers, toys, flowerpots, or any other containers.
- Remove/destroy discarded tires, bottles, cans, pots and pans, and broken appliances, or anything that holds water.
- If you are going to be traveling, check before leaving if chikungunya is a problem at your destination, and if so, be sure to take precautions against mosquito bites. For country-specific travel information and recommendations, visit the Center for Disease Control (CDC).
Information for Clinicians
Disease reporting
Chikungunya is notifiable in Hawaii and should be reported by telephone to the Disease Outbreak Control Division, Disease Investigation Branch on Oahu, or to the District Health Office on the neighbor islands as soon as a provisional diagnosis is established.
Disease Reporting Phone Numbers (24/7)
Oahu (Disease Investigation Branch): (808) 586-4586
Maui District Health Office: (808) 984-8213
Kauai District Health Office: (808) 241-3563
Big Island District Health Office (Hilo): (808) 933-0912
Big Island District Health Office (Kona): (808) 322-4877
After hours on Oahu (Physician’s Exchange): (808) 600-3625 or Toll Free 1-800-360-2575
After hours on neighbor islands: (800) 360-2575 (toll free)
The State Laboratory Division (SLD) of HDOH can perform several different tests for Chikungunya. The real-time reverse transcriptase polymerase chain reaction (rRT-PCR) and serologic (immunoglobulin M [IgM]) testing can be done by SLD. Any positive or equivocal IgM result requires follow up testing by plaque-reduction neutralization test (PRNT), currently only available through HDOH at the Centers for Disease Control and Prevention (CDC). All specimens should be routed to SLD through a certified clinical laboratory.
Healthcare providers submit the specimens to SLD along with the completed Clinical Specimen Submission Form (SLD Form 81.3). All testing requires HDOH review and approval. If healthcare providers pursue testing through a private commercial lab, consult clinical laboratory for send-out options. Healthcare providers should follow CDC testing criteria for whom to test and guidance for what should be tested
Additional Resources
Centers for Disease Control and Prevention (CDC)
State Laboratory Division (SLD) Test Menu
Trioplex (Zika, Dengue, Chik) Real-Time RT_PCR
Last reviewed August 2022