Carbapenem-Resistant Enterobacterales (CRE)
About This Disease
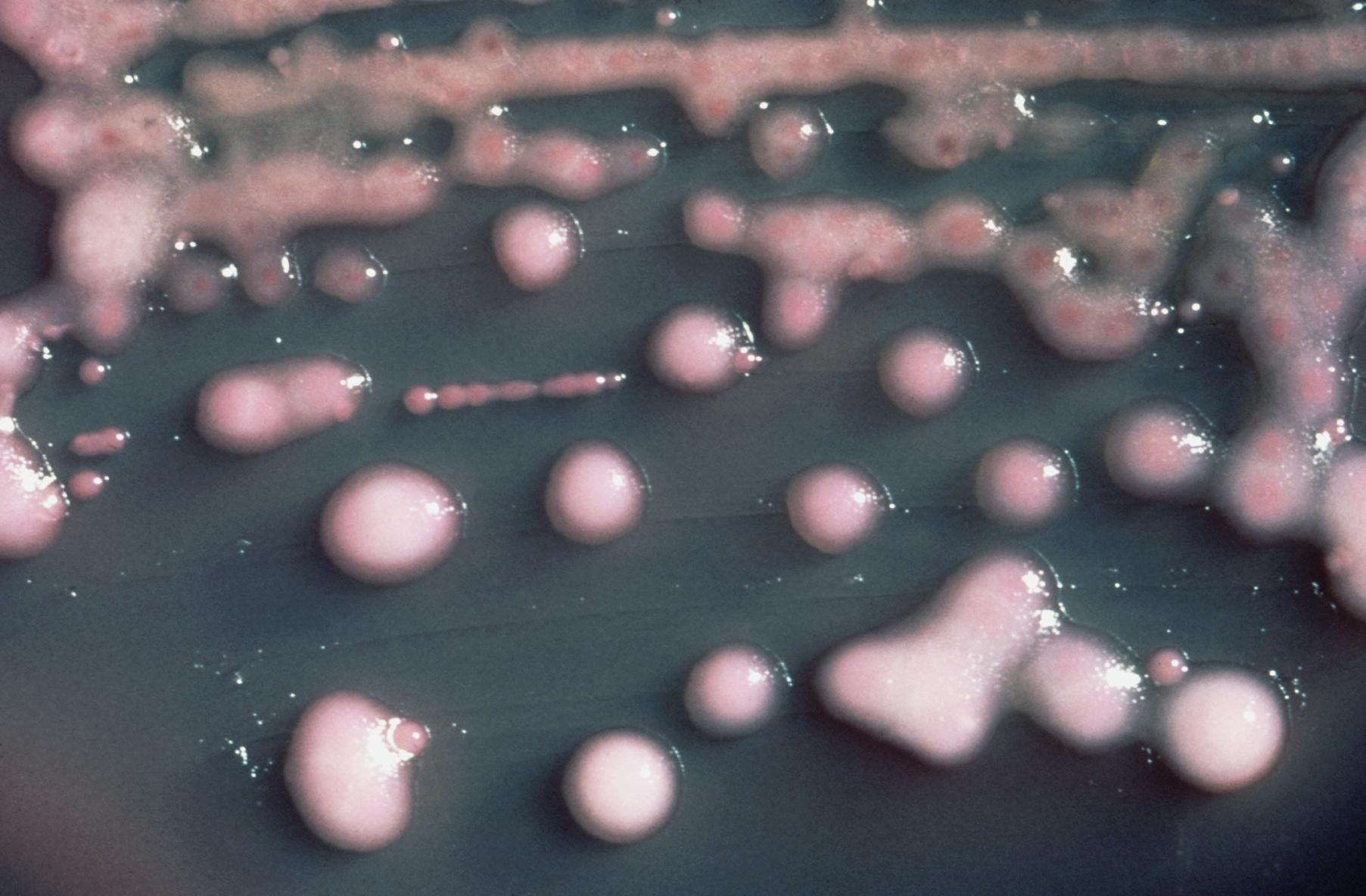
Carbapenem-resistant Enterobacterales (CRE), formerly Enterobacteriaceae, are a family of bacteria that are resistant to carbapenem class antibiotics. Carbapenem is a type of broad-spectrum antibiotic frequently used to treat life-threatening severe infections. Antibiotic resistance occurs when the antibiotic no longer works on the bacteria it was designed to kill. Resistance to carbapenems can develop due to different mechanisms, but one of the more common ways that Enterobacterales become resistant to carbapenems or any other antibiotic is due to the production of carbapenemase enzymes. One particular enzyme first identified in the United States around 2001, Klebsiella pneumoniae carbapenemase (KPC) breaks down carbapenems and makes them ineffective. Other carbapenemase enzymes, such as New Delhi Metallo-beta-lactamase (NDM), Verona Integron-Encoded-Metallo-beta-lactamase (VIM), Imipenemase (IMP), and Oxacilliniase-48 (OXA-48) also breakdown carbapenems, leading to the development of CRE, but are not as common in the United States as KPC.
Signs and Symptoms
Enterobacterales are commonly found in normal human intestines (gut). Sometimes these bacteria can spread outside the gut area and cause serious infections such as pneumonia, meningitis, bloodstream infections, urinary tract infections, and wound infections. . A CRE infection causes similar symptoms you would get with any other bacterial infection, including fever, redness, swelling, or pain at a specific site if a wound is infected.
Transmission
To get a CRE infection, a person must be exposed to CRE bacteria. Persons who are infected or colonized with CRE bacteria may be a source of transmission to others. CRE bacteria are most often spread person-to-person by coming into contact with wounds or stool, or from infected or people colonized with a CRE. CRE can cause infections when they enter the body through medical devices like catheters, ventilators, or through wounds caused by injury or surgery.
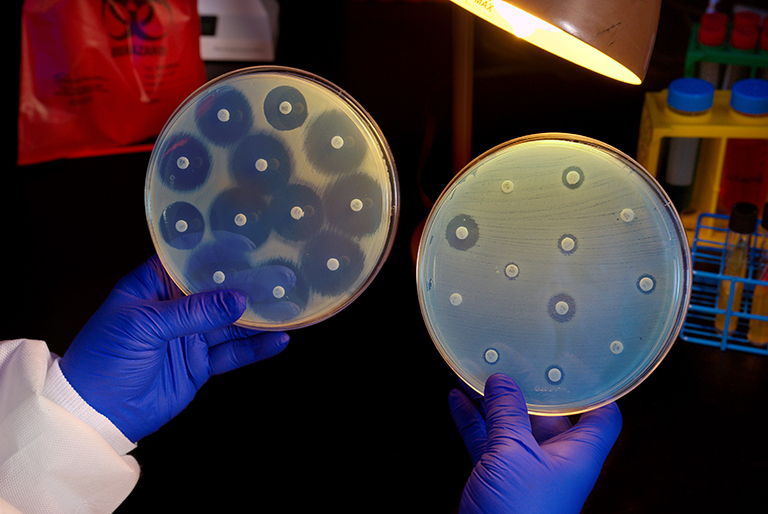
Diagnosis
If you have an infection associated with an Enterobacterales, your healthcare provider may order additional tests to determine if it is resistant to antibiotics.
Treatment
CRE are often resistant to many commonly prescribed antibiotics but may remain susceptible to one or more antibiotics. Decisions on treatment of CRE infections should be made on a case-by-case basis by a healthcare provider. Some people might be colonized rather than infected with CRE and may not require any treatment.
Risk in Hawaii
Enterobacterales are one of the most common causes of bacterial infections in both healthcare and community settings. Examples of Enterobacterales are Escherichia coli (E. coli), Salmonella enterica, and Klebsiella pneumoniae. CRE infections are most commonly seen in people with exposure to healthcare settings like hospitals and long-term care facilities, such as skilled nursing facilities and long-term acute care hospitals. Patients who are taking long courses of certain antibiotics, and those who require ventilators or catheters are among those at highest risk for a CRE infection. Hawaii is still a relatively low incidence state. For information about the different types of CRE in the United States, visit the CDC webpage, Tracking CRE in the United States.
Prevention
To prevent CRE infections, patients should:
- Expect all doctors, nurses, and other healthcare providers to wash their hands with soap and water or an alcohol-based hand rub before and after touching your body or tubes going into your body. If they do not, it is okay to ask them to do so.
- Tell your doctor if you have been hospitalized in another facility or country
- Take antibiotics only as prescribed by your healthcare provider
- Practice good hand hygiene and wash your hands often:
– Before and after changing wound dressings or bandages
– After blowing your nose, coughing, or sneezing
– Before preparing or eating food
– After using the bathroom - Ask questions. Understand what is being done to you, the risks and benefits.
Additional Resources
Hawaii State Department of Health CRE Fact Sheets (PDF) :
English | Chuukese | Ilokano | Japanese | Marshallese | Tagalog
Centers for Disease Control and Prevention (CDC)
Healthcare Associated Infections (HAI) Patient Empowerment Flier
Learn about Handwashing
Information for Clinicians
Clinicians play a critical role in slowing the spread of CRE. Rapidly identifying patients colonized or infected with these organisms and placing them on strict Infection Control Precautions when appropriate, using antibiotics wisely, and minimizing invasive device usage are all important parts of preventing CRE transmission
CDC has developed a CRE toolkit for facilities to control CRE.
Last reviewed August 2022